July 24, 2023
– By Debbie Quinn –
ENI partner communities and their Advisory Groups answered questions about health in their communities. As our team looked at their answers, it was clear there were a few health issues that were of major concern in every community. ENI will begin to address these concerns through a Health Equity Plan for each community. We’d also like to highlight some of these concerns here to build capacity to deal with the health and quality of life challenges of tomorrow, starting today.
This month, we’ll discuss DIABETES, which is prevalent across the U.S. Over a half million people in Alabama have been diagnosed with diabetes, which is a long-term, non-curable disease. According to the Centers for Disease Control and Prevention (CDC), “more than 37 million people in the U.S. have diabetes, and 1 in 5 of them don’t know they have it.” Research published by the National Institutes of Health states that type 2 diabetes “disproportionately impacts U.S. racial and ethnic minority communities and low-income populations,” and these populations have higher rates of diabetes-related complications. However, diabetes can affect people of any race, income bracket or age.
What is Diabetes?
According to the CDC, “diabetes is a chronic (long-lasting) health condition that affects how your body turns food into energy.” You want to try and manage it as best as you can, but that comes with changes to your lifestyle, medication and meal planning.
The food we eat becomes glucose (an easily digestible form of sugar) in our stomach and intestines. Glucose mainly comes from carbohydrates in food and drinks. According to the Cleveland Clinic, glucose is your body’s go-to source of energy, so we do need a healthy amount of glucose. Your blood arteries and veins carry glucose to your body’s cells to use for energy.
When everything is working properly, glucose is absorbed into your bloodstream to feed your heart, eyes, blood vessels, nerves, etc., with vitamins, proteins, and energy. Each part of your body and organs takes what it needs.
People who have diabetes have a deficiency in INSULIN that disrupts the cycle of feeding your body, causing too much glucose to stay in your bloodstream. Diabetes is considered one of the “Silent Killers”. That means the symptoms slowly add up, and by the time you realize you have the disease, it has already caused damage to the parts of your body that didn’t get the particular ‘food’ they needed. Early diagnosis is important to control damage to your body. If you are diagnosed early, it’s less likely that damage from too much glucose will occur.
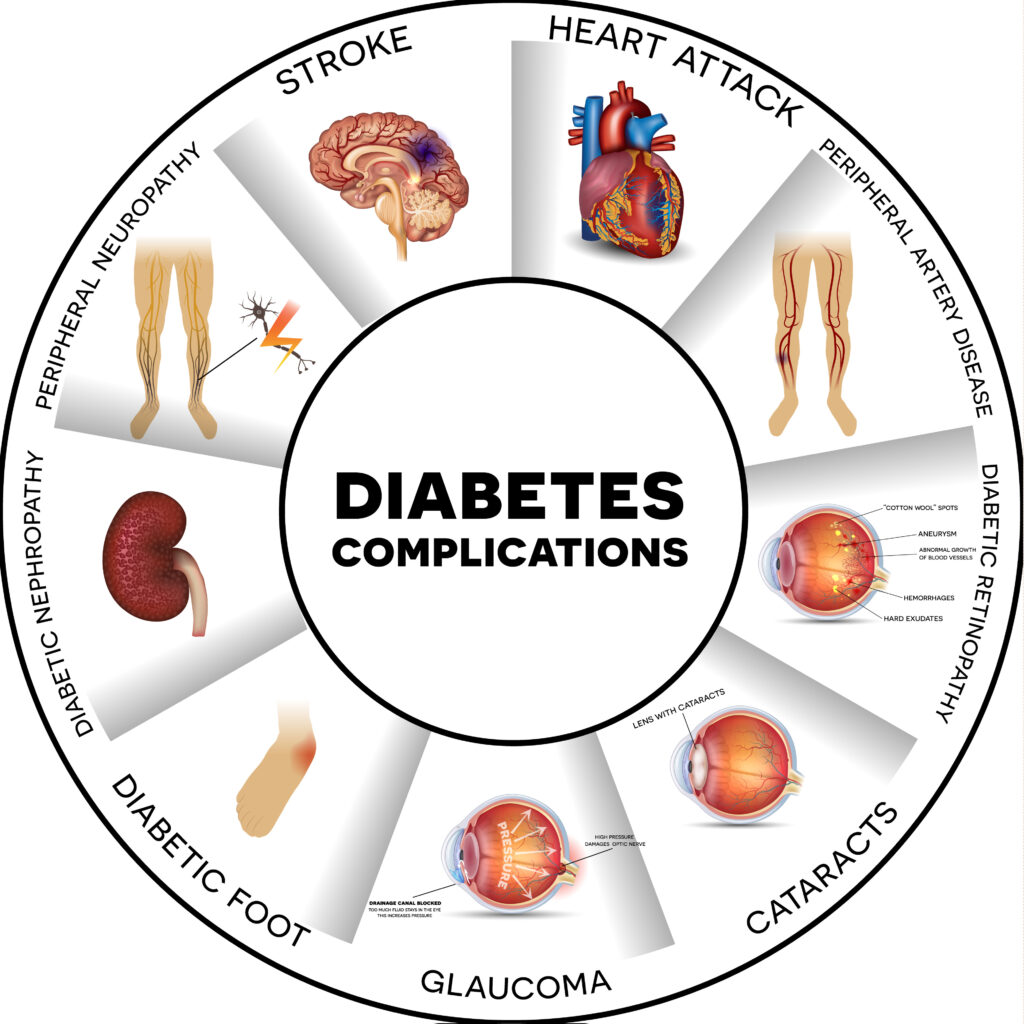
Diabetes affects your whole body. As the illustration above shows, too much or too little sugar can lead to complications that damage just about everything in your body. Major symptoms of diabetes include:
- Always thirsty
- Increased hunger
- Frequent urination, especially at night
- Blurry vision
- Extreme tiredness
- Sudden weight loss
It’s important to talk to your healthcare provider if you or a family member have any of these symptoms.
Managing Diabetes
Diabetes can be managed to delay or prevent health complications. Here are six important tips for managing diabetes.
1. Blood sugar monitoring
According to the Cleveland Clinic, “monitoring your blood sugar (glucose) is key to determining how well your current treatment plan is working. It gives you information on how to manage your diabetes on a daily — and sometimes even hourly — basis.” Monitors are available from your health care provider along with all the basic needs for finger sticks or a continuous glucose monitor (CGM). With consistent checks, you and your healthcare provider can determine the best range to keep your blood sugar.
2. Meal planning
A healthy diet is key to managing diabetes. If you take insulin, counting the carbs you consume is a large part of management. The amount of carbs you eat should coincide with how much insulin you take.. An added benefit of weight management is a reduction of your potential risk for heart disease.
I have several friends who think, “I’ll eat that extra piece of cake, drink that wine and just give myself more insulin.” Remember, your body is not breaking down sugars adequately so the body can use them properly. Taking more insulin than what the doctor prescribed is bad for your organs and tissues.
As you plan, remember that nothing is completely off-limits. You won’t get diabetes from enjoying small amounts of sweets occasionally. Talk to your diabetes team to make a plan that’s best for you.
To get you excited about a healthy diet, watch KevOnStage discuss simple tips for eating healthier on a budget and a busy schedule. The CDC also offers tips for meal planning for diabetics.
In the videos below, Dr. Onikia Brown, Associate Professor in the Department of Nutritional Sciences at Auburn University, overviews nutrition-related health disparities. Dr. Brown also provides tips for making healthy choices and building healthy eating habits.
3. Exercise
Maintaining a healthy weight is important for people with diabetes, even though a healthy weight might mean something different for everyone. According to the Cleveland Clinic, keeping A1C levels (a blood test that indicates pre-diabetes or diabetes) below 7% may help people reduce the risk of complications from diabetes. According to the CDC, being active makes the insulin you take work better in your body to create energy. If you exercise routinely, your body may not need as much insulin. Fat storage increases when using insulin, especially around the mid-section of your body. Regular exercise is an important part of management for all people with diabetes.
4. Mental health
Living with diabetes can also affect your mental health. According to the CDC, people with diabetes are two to three times more likely to have depression than people without diabetes. Diabetes can be a lot to manage, along with family, work, kids, school, and other life stressors. Stress is sometimes unavoidable, but lots of stress can make managing diabetes harder and takes a toll on your body.
With depression, the feelings of sadness and loss of interest in activities you used to enjoy can get in the way of how well you function at work and home, including taking care of your diabetes. The risk for complications like heart disease and nerve damage can go up when diabetes is unmanaged.
A large percentage of people with diabetes who have depression go undiagnosed. But treatment for mental health is effective, and left untreated, depression often gets worse. Communication with family, neighbors and friends, 30 minutes of physical activity, and relaxation exercises, can help with your mental health. Talk to your diabetes team about ways you can manage stress.
5. Smoking
According to the CDC, smoking is associated with the development of diabetes. The more someone smokes, the more likely they will develop diabetes and have problems managing their insulin and diet. When you smoke with diabetes, it might put you at risk for additional diseases. People with diabetes who smoke have an increased risk for heart disease, kidney disease and eye damage. Diabetes can also lower the blood flow to the legs and feet and cause nerve pain in feet, arms and legs. Low blood flow in the arms and legs can lead to infections, ulcers and eventually amputation.
6. Emergency preparedness
Be prepared for the next emergency if you have been diagnosed with diabetes. In addition to the typical items you need in an emergency, it’s also helpful to have a diabetic tool kit on hand. Your kit could be essential during emergencies, evacuations or trips so that you are prepared for up to three or more days with what you need. Consider including the following items in your kit:
- A small cooler with re-freezable ice to keep your insulin cold
- Needles and syringes for your insulin and an empty soda bottle for your needles after use
- Anything you use to treat hypoglycemia (low blood sugar) like sealed orange juice or glucose tablets
- Batteries for your glucose monitor
- Phone chargers
- Your diabetes diagnosis and recent lab test showing your A1C, kidney and liver functions
You can live a healthy life with diabetes. Lifestyle changes and your food choices matter a lot. Be sure to talk to your diabetes team to craft a plan that works for you.


